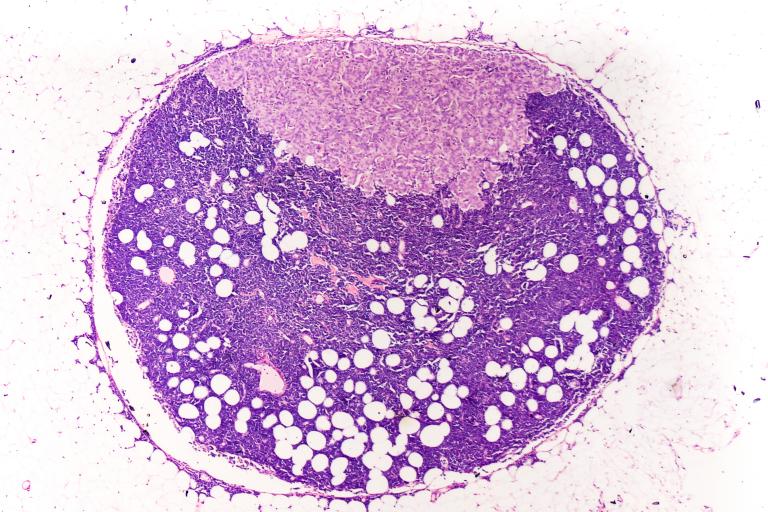
The sentinel nodes are the first few lymph nodes to which a tumour drains. Sentinel node biopsy involves injecting a tracer material that helps the surgeon locate the sentinel nodes during surgery. The sentinel nodes are removed and analysed in a laboratory, while leaving the rest of the lymph nodes in the area alone.
Sentinel lymph node biopsy helps to direct on-going care because it is the most predictive factor for the risk of spread of your melanoma. If your biopsy is negative, you are at a lower risk of spread of your melanoma and your follow up can be tailored to take this into consideration, including less intensive investigations and follow up.
If a sentinel lymph node biopsy reveals spread of your cancer, your doctor might recommend additional scans, more frequent reviews to check on your progress and may advise on further management, including possible surgery, medications or post-operative radiotherapy, depending on the nature of the cancer and your needs. This is often undertaken as part of a specialist Melanoma multidisciplinary team review. We are very used to helping patients to navigate this process and will take time to answer your questions so you are properly informed about your diagnosis, management and what it all means.